There are two kinds of people in this world, those who like and make New Year’s resolutions, and those who think that New Year’s resolutions are pointless and should actually be renamed as “things you try to do all year but give up on by February”. I myself however, am somewhat in the middle of these two kinds of people (much like I am on the whole Marmite debate. I don’t love it, nor do I hate it. I am truly indifferent…WHAT DOES THIS MEAN).
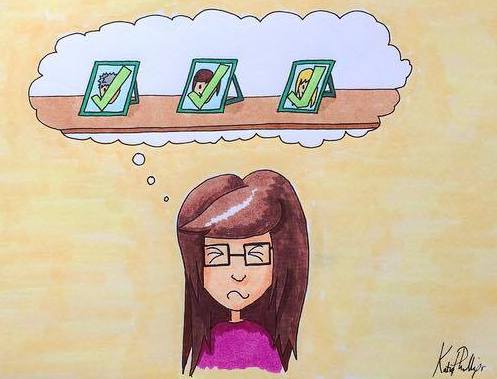
I actually like the idea behind New Year’s resolutions. I think it is good to see the new year as a chance to improve on whatever happened in the previous one, see it as a fresh start and a clean slate without all the baggage you have dragged around for the past twelve months. That said, I have not made a New Year’s resolution myself since 2010, and that is because I feel that when people make these promises to change, they are far too ambitious and unattainable. They set themselves tasks like “fly to the moon” or “play tennis at Wimbledon” when they haven’t yet thought to apply to astronaut school or pick up a racket. Back in 2010 I made three new years resolutions, those being:
- Be happy all the time
- No anorexia
- No OCD
As midnight approached I felt a surge of excitement. The moment that clock chimed (lets pretend we still live in a time where it is common to have a grandfather clock that chimes..it is a nicer image than me staring at the digital numbers on my phone waiting for 23:59 to become 00:00), my life was going to change, I was determined, and I had made a promise to myself that 2011 was going to be better. Then it happened. The clock struck midnight, and suddenly my carriage that had brought me to the party turned into a pumpkin and I lost a glass slipper!…Wait..no sorry…got mixed up in the life of someone else a little…no, what actually happened was the clock struck midnight and I felt a weight fall from my shoulders (much like a glass slipper was slipping from the sole of a future princess…)
Finally 2011 was here and I was recovered, I never had to do an OCD ritual again, I could eat and I would be smiling for the rest of my life. Looking back I can’t believe I was so deluded, but the first thing I did in 2011 was to run to the bathroom to wash my hands once, just to prove that I was in control again and could stop easily after one squirt of soap. But I didn’t stop. After the squirt had been collected in to my hands my thoughts immediately burst in and I found myself rubbing my hands together vigorously with the same urgency as I had done in 2010. I became incredibly stuck, thoughts flying so rapidly that before I knew it a significant amount of time had passed, over 100 squirts of soap had been used and the only thing I could see through the tears of despair and frustration was a basin full of bubbles. As I went back downstairs to join the others still milling around drinking champagne and watching the odd late firework banging about in the distance, I felt totally defeated. I had failed. I hadn’t even kept my resolution for 24 hours before engaging in the behaviours I told myself I was finished with, and my hopes for change fizzled out like an old sparkler. Granted I was being a bit dramatic by seeing the whole year as ruined and giving up because of one ritual, but logically because of the strict boundaries of “No” OCD, I had in essence failed, so what was the point carrying on? Clearly recovery was impossible.
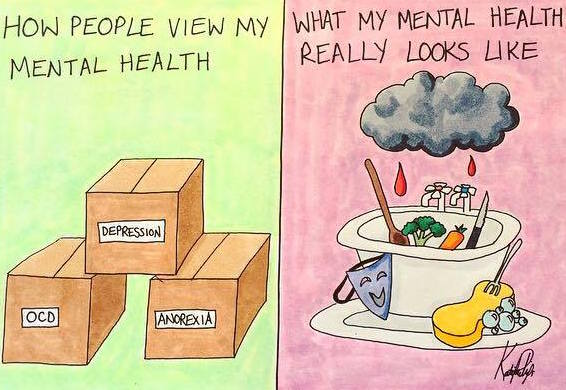
It is only now looking back that I realise that the problem with my resolution and the reason I had “failed” was entirely the wording and dramatic nature of the resolution I had made. I didn’t set myself a manageable goal of trying to reduce the amount of time in the shower over the course of the year or anything reasonable, a goal that would focus on steady progress with potential slip ups yet still a continuous effort to push forward. Instead I had set myself the impossible task of transforming from a person who had been dominated by mental health problems for the last 7 years to a “normal person” in less than 7 seconds, which is pretty much like someone setting the goal of “flying to the moon” without realising all the steps it takes to get to that point.
Admittedly, I have always struggled with people telling me to “take things steady” and “take baby steps” when it comes to recovery. I am a very black and white person, either I am better or I am not, “baby steps” and little goals like “exercise for five minutes less per day” do not help me. I want total freedom from this mental health cage, not just the same cage with an ocean view.
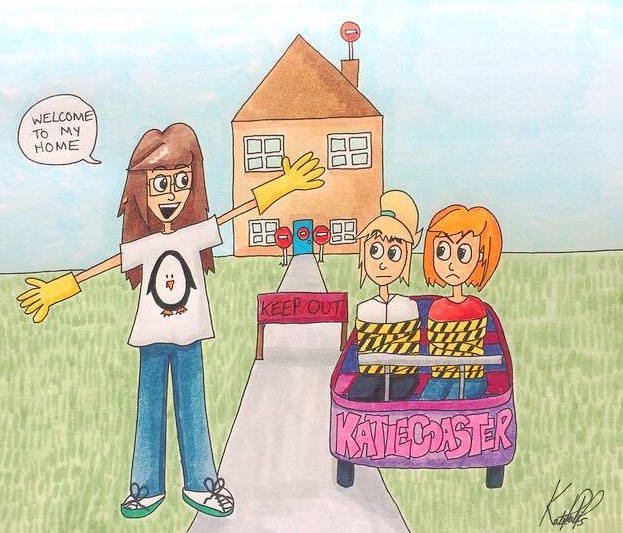
However, my attitude to all this recently underwent a bit of refurbishment when I was glancing through pictures on Facebook and stumbled across a photograph that I posted online in 2014 to commemorate the fact that I had graduated from university, and for the first time, as I looked at the picture, taking “baby steps” made some sense.

As you can see this picture is a comparison shot between little 4 year old me on my first day of school, and 22 year old me graduating from university after a rocky 18 years bumbling through the education system (I look pretty happy in that picture but that was because my mum took it before I found out I wasn’t allowed to keep the funny hat and gown. That was a major disappointment. The only thing I got out of that day was a piece of paper saying I had a theology degree. Who the hell wants that? I didn’t go to university to be educated, I went for the damn hat!)
Looking at these pictures it is very black and white. In one I have a degree (and a marvellous hat), and in the other, I have no degree (and no hat. 4 year old Katie had a hard life). That said, though there is a stark difference in achievement between those two pictures, it isn’t because I made a grand resolution at the age of 4 that changed my life in a second. When I was 4, the thought of getting a degree one day had not entered my mind.
Imagine if someone went back in time now, found little 4 year old me and said “go and get a degree in theology this year”. I would probably have cried (and asked what the hell theology was). When I was 4 there was no way I could just go off and get a degree. I had birthday parties to plan for my teddy bears, letters to write to Santa and hopscotch competitions to attend! I couldn’t tie my shoes yet let alone write essays on Saint Thomas Aquinas or Augustine of Hippo (genuine name…Hippo…it has been years but I am still amused), so setting that goal for me at age four would have been overly ambitious and basically would have set me up to fail.
Had this time travelling person told me to go to school that day however instead of getting a degree right then and there, I would have probably looked at them, nodded and then got on with it. When doing so I wouldn’t have realised that me turning up for a morning of finger painting was actually the first part of my journey to that oh so lovely yet tragically temporary hat (and a degree I am now stuck with forever), but it was. Without achieving all those little steps in-between, the sports days, the story books and the words of wisdom over the years, I would never have got that degree (actually maybe cancel the sports day bit..I don’t think they were particularly important…).
My 2010 new years resolutions to totally recover in the blink of an eye then, were basically the equivalent of me telling 4 year old Katie to go and get a degree before the little tike had learned to read, and it is in realising this that I can see the value in making new years resolutions, as long as they are the baby steps to get you to your goal rather than a leap to success that no Olympic long jumper could make even with a springboard.
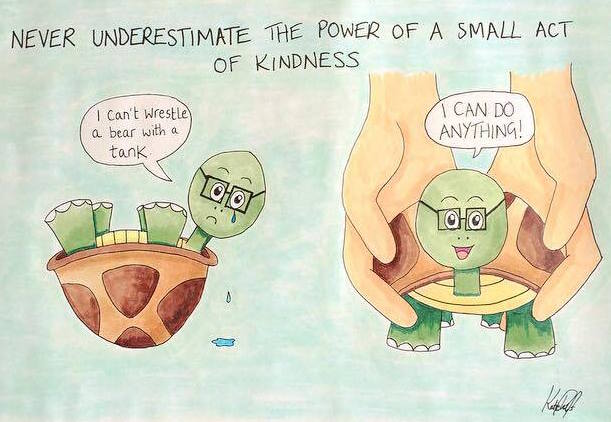
If you want to set yourself a resolution for 2017, make a resolution that you can do over time, that allows for mistakes and gradual progress rather than instantaneous results. If you want to recover completely from OCD, make your goal to try and reduced the number of times you get caught in rituals over the course of the year. If you want to recover from depression don’t set the goal of being happy all the time, simply think about the things that could one day make you happy and go out trying to achieve them, even if that goal is just phoning up to enquire about a course. It is the same with progress in eating disorder behaviours as well as any other mental health condition, and though admittedly it takes a lot longer than the midnight miracle method I wished for in 2010, I think it is the only way to make it through this journey.
My hope in life is that one day I will be able to take a picture as someone who is no longer struggling with mental illness and to see it alongside that 4 year old me as a sign of how far I have come in ways other than education, and working towards that is my goal for the next twelve months. 2017 is not going to be “my year”, the year I change, recover totally and get a brand new life, but it is another year in which I will continue my 2016 resolution of doing all I can, listening to professionals, talking and attending all appointments, to one day make that massive goal of recovery. Taking my medication this morning has not made me better, but hopefully it is a baby step along the way.
Happy New Year everyone x