Every mental health problem has a troubling mist of stigma surrounding it, but recently I have noticed that not all stigmas are created equally, and often the level of judgement varies depending on what condition that judgment is focused on.
It isn’t even as simple to organise as “personality disorders get this level of stigma and mood disorders get this level”, because the amount of stigma can vary even between conditions of the same category, especially, I have noticed, when it comes to eating disorders, more specifically, anorexia, bulimia and binge eating disorders.
I am sure there are exceptions out there but as a broad overall in my experience, I have found that the stigma surrounding bulimia and binge eating disorder (henceforth referenced by its acronym BED), is a lot worse than that existing around anorexia, and considering they are both so similar in being considered under the umbrella category of eating disorders, it makes me wonder why that is.
I hate to say it but the level of judgement isn’t even exclusive to people who don’t know anything about mental health, and I have found it is incredibly prominent in the world of eating disorder sufferers themselves.
For example, over the years in various groups and hospitals, I’ve met a lot of people with anorexia and I have found that many of those people actually had the fear of becoming bulimic or having BED as one of their reasons to fear recovery from their anorexia. I even remember one particular incident in treatment where a new patient asked another patient if their eating disorder was bulimia and the insinuation that that could be the case was taken as extremely offensive. Obviously it isn’t exactly polite to go wandering around introducing yourself by asking people intrusive questions about their mental health, but that wasn’t the part of the question that was taken as offensive, it was the bulimia part, and I know for a fact that had the question been “do you have anorexia?” the reaction would have been more “yes I do but blimey that is a bit outright as a question, we haven’t even had a cup of tea together yet” rather than “how very dare you accuse me of such a thing”.
I suppose in life it is common to fear the unknown, so it is more likely you will fear something that you haven’t experienced as opposed to something you live with everyday.
For example I used to be terrified of blood tests but now I have them every few weeks and am not scared of them at all. Indeed I am quite the professional and can now have blood taken whilst remaining perfectly relaxed and without so much as a shudder (as long as that blood is being taken by a professional using one of those syringe things…I don’t mean I am cool with having people stop me in the street and attack me with a chainsaw…I imagine that would result in quite a lot of shuddering so please do not do that to test my statement because I will certainly shudder and you will certainly get arrested).
Still, as much as that would make sense for people who don’t already have eating disorders, it seems a bit odd for someone who is familiar with the life of living with an eating disorder that is trying to kill you, being so scared of basically an eating disorder trying to kill you with a different name. It’s a bit like the experience of having a tabby cat, living with a tabby cat, yet still fearing ginger cats when really it is the exact same thing only with a slightly more tangerine-esque glow.
I actually don’t think the fear of the unknown is really a part of the increased stigma around bulimia or BED versus anorexia at all though, rather I think it has to do with the fact that so many traits and behaviours that are associated with anorexia are praised in society.
Despite the fact that not all people with anorexia are underweight and, contrary to popular belief, people with anorexia DO eat, as a general consensus, people associate being anorexic with losing weight, being thin and never letting a morsel pass your lips, three things that are seen as good by most people.
Think about it, when it comes to all of those diet clubs out there like Slimming World and Weight Watchers, you get things like certificates and “I lost half a stone” keyring prizes for losing weight and I am pretty sure they only hand out certificates in life for things that you are supposed to be proud of. When I was learning to swim as a child at least, they certainly didn’t hand out prizes for the person who was drowning in the bottom of the pool (which is understandable as that is not exactly the aim of a swimming lesson but still a bit sad as it is the person who was drowning at the bottom of the pool who could use a bit of cheering up with a certificate, as opposed to the person who managed to swim a perfect ten lengths of front crawl…what do they need cheering up for? Isn’t it enough not to have water up your nose? Kids today are so ungrateful!).
Similarly, as I have mentioned before, in society we have this weird obsession with associating refusing a piece of cake at a birthday party as “being good”, while those of us with icing on our chins are doing something “naughty”, so the idea that anorexic people don’t eat unhealthy foods is similarly admired, rather than feared as a sign that someone is potentially starving themselves to death.
Anorexia is often seen as a sign of strong self control, whereas bulimia and BED on the other hand is associated with things like a lack of control and even more infuriatingly, greed/gluttony. These two things are so opposite to being admired that they are two of the seven deadly sins for goodness sake, and it drives me up the wall, back down round Tottenham and up the wall all over again because neither bulimia nor BED are anything to do with greed or gluttony. I am seriously considering getting that as a bumper sticker so that at least whilst I am doing all this being driven mad I am educating people along the way, although I would really rather not drive at all because I do not have a license and petrol is incredibly expensive.
If a person with bulimia or BED goes around a supermarket and buys a lot of unhealthy food to binge on or eats excessive amounts to the point that they are compelled to purge (or not), it is not out of personal want or greed, it is because they have an eating disorder in their head that drives and compels them to do so. It is not the person with the disorder in control thinking “ah this will be a lovely way to spend an evening, I thoroughly enjoy a few hours weeping into a toilet with a throat as raw as sandpaper”, it is the disorder that is at the steering wheel, and when people are attempting recovery it is more about learning to steal that control back from the disorder rather than trying to control their personal desires.
Similarly, anorexia is nothing about self control and I would even argue shows an extreme lack of control. You can praise people for not dunking a hob nob in their morning cuppa all you like, but how in the hell is it a sign of good self control to be incapable of eating and starving yourself to death? Who would give a certificate out for that? (I realise this may sound hypocritical considering I was arguing that we should give prizes to people drowning in a swimming pool five minutes ago but let’s just set that example aside for the time being…). Much like the person with bulimia, when I struggle to eat I do not feel in control of the situation and I do not look forward to an evening crying over a bowl of cereal, excitedly clapping my hands at the prospect of a few hours staring at a Weetabix.
Bulimia, BED and anorexia then are, despite the varying stigma, very much the same and very similar in that they are about wrestling with a deadly eating disorder. That’s it. It doesn’t matter that two of the disorders are known for expressing themselves via binging and possibly purging, whereas the other has its name up there as a sign of a lot of lettuce and weight loss. Aside from the treatment required, the expression of the disorder has nothing to do with it just as the colour of a ginger cat means nothing next to the tabby, THEY ARE BOTH JUST CATS AND BULIMIA/BED/ANOREXIA ARE ALL EATING DISORDERS. Both bulimia and BED are as much about greed as anorexia is about self control, aka they have nothing to do with it, and I really think we need to spread that message to stop the level of shame surrounding such disorders.
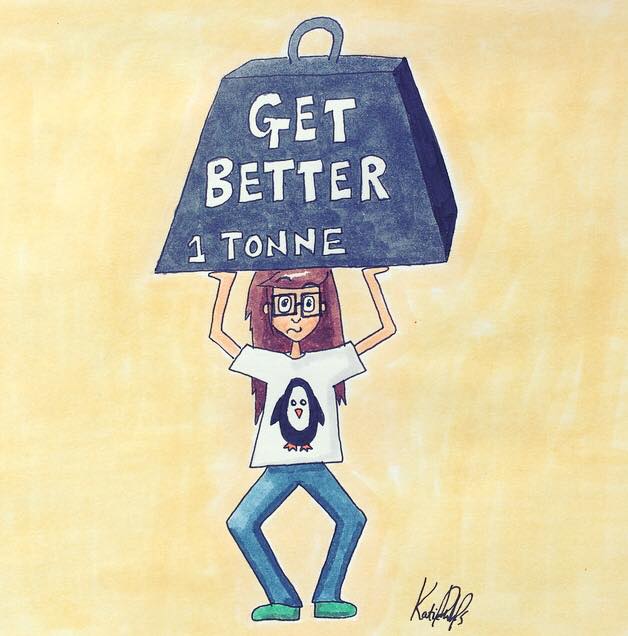
Admitting you have an eating disorder is hard and embarrassing, but it is even harder and even more embarrassing when you have extra stigma piled on top just because of the name of your condition. If bulimia and BED are portrayed as about greed and shame, people are far less likely to admit to having a problem and seek help which is incredibly dangerous as both disorders are serious, they are deadly and can be fatal with complications caused by things like electrolyte imbalances, heart attacks and other consequences of recurrent purging, so seeking support for these conditions is as important as seeking help for any restrictive disorders. We need to stop the judgement and discrepancies between different names for eating disorders and need to see them back under the same deadly umbrella, they are ALL serious, ALL dangerous, and ALL are worthy of the help and support needed to get better.
Take care everyone x